Research Themes
The BioMimetic Systems Engineering (BMSE) Lab combines experimental and computational methods in tissue engineering, bioimage analysis, and computational biology to characterise blood and blood vessel growth and disease processes. Experimental methods include biomaterial fabrication, bioreactor and microfluidic chip engineering, stem cell & tissue isolation, haematopoietic and angiogenic cultures, imaging and cytokine analyses, and more. Computational methods include microscopy and medical image segmentation, co-localisation, shape analyses, and predictive models of cell populations (differential equations), single-cells (agent based), and tissue biomechanics (finite element). Currently-running projects include:
Diagnostic Culture Models to Screen Graft Versus Host Disease
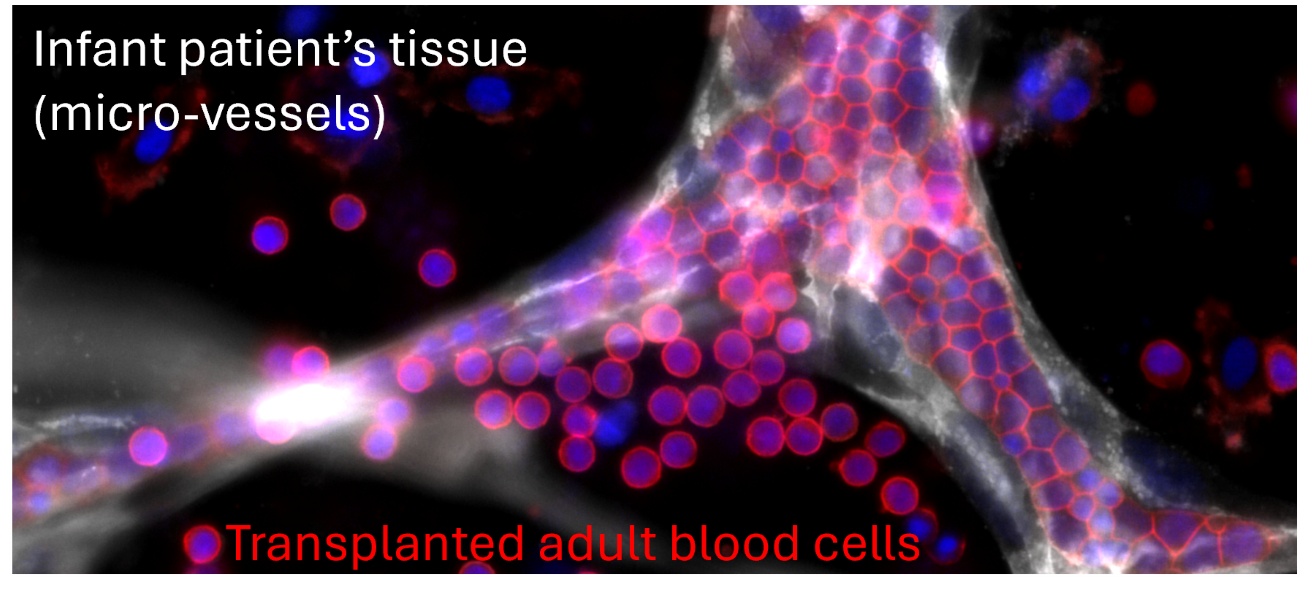
Bone marrow and organ transplants have been a lifesaving option for 200,000 patients per year. Patients and infants in need of blood, stem cells or solid organs often rely on donations from unrelated donors, despite their substantial risk of graft versus host disease (GVHD) which may lead to transplant rejection. By using rare stem cells from donated blood units, this project aims to engineer cell culture models which can accurately predict whether a patient would negatively react to a specific donor's cell or organ transplant, providing insights which could save thousands of Australian lives.
Researchers: Rose Ann Franco (Lead), Sara Chiaretti. Partners: Australian Red Cross Lifeblood, Queensland Cord Blood Bank at the Mater Hospital. Funding: Australian Research Council, Ramaciotti Philanthropy, UQ Internal Funding.
Bone Marrow Mimicry Bioreactors for Blood Cell Therapy Manufacturing

Cell therapies are widely considered to be the next step-change in clinical medicine, curing previously uncurable disease. However, many cell therapies cost $100,000 to $3,000,000 per dose, an expense which patients and healthcare systems cannot afford. If we could manufacture lab-grown cell therapies as efficiently as our body does, we could reduce the cost of cell therapies 10x-100x and deliver more curative treatments to more patients in need. Specifically, we are using our body's bone marrow as an inspiration for growing blood cell therapies such as blood stem cells (HSPCs) and red blood cells (RBCs).
Researchers: Astrid Nausa Galeano (Lead), Rose Ann Franco, Susana Costa Maia. Partners: Australian Red Cross Lifeblood, Queensland University of Technology, University of Maastricht. Funding: Australian Research Council, Ramaciotti Philanthropy, UQ Internal Funding.
High-Content Microphysiological Systems for Cell Culture Screening
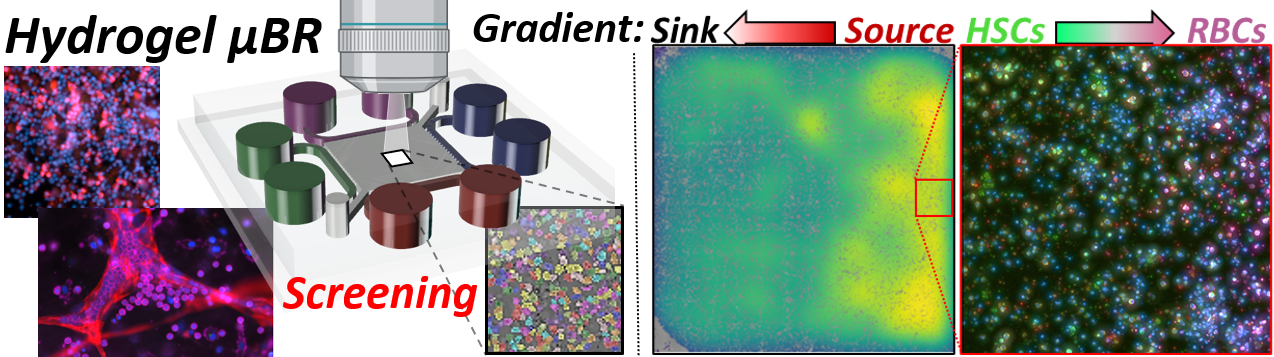
3D culture systems can grow greater numbers of higher-quality cells at lower costs than traditional liquid suspension or 2D cultures, however the adoption of 3D culture systems in biopharmacuetical industries remains limited due to current dependenance on culture high content screening (HCS). Our lab is engineering the first experimental platforms and compuational models to preform HCS on 3D cell cultures for process optimisation and drug screening. Specifically, we are engineering live-imaged high-throughput hydrogel microchip platforms to optimise stem cell expansion and angiogenesis.
Researchers: Ryan McKinnon (Lead), Rose Ann Franco, Ashley Murphy. Partners: Queensland Cord Blood Bank at the Mater, Royal Brisbane & Women's Hospital Dept of Haematology, Queensland University of Technology. Funding: Australian Research Council, Ramaciotti Philanthropy, UQ Internal Funding.
Additive Manufacturing to Predict Patient-Specific Cardiovascular Disease
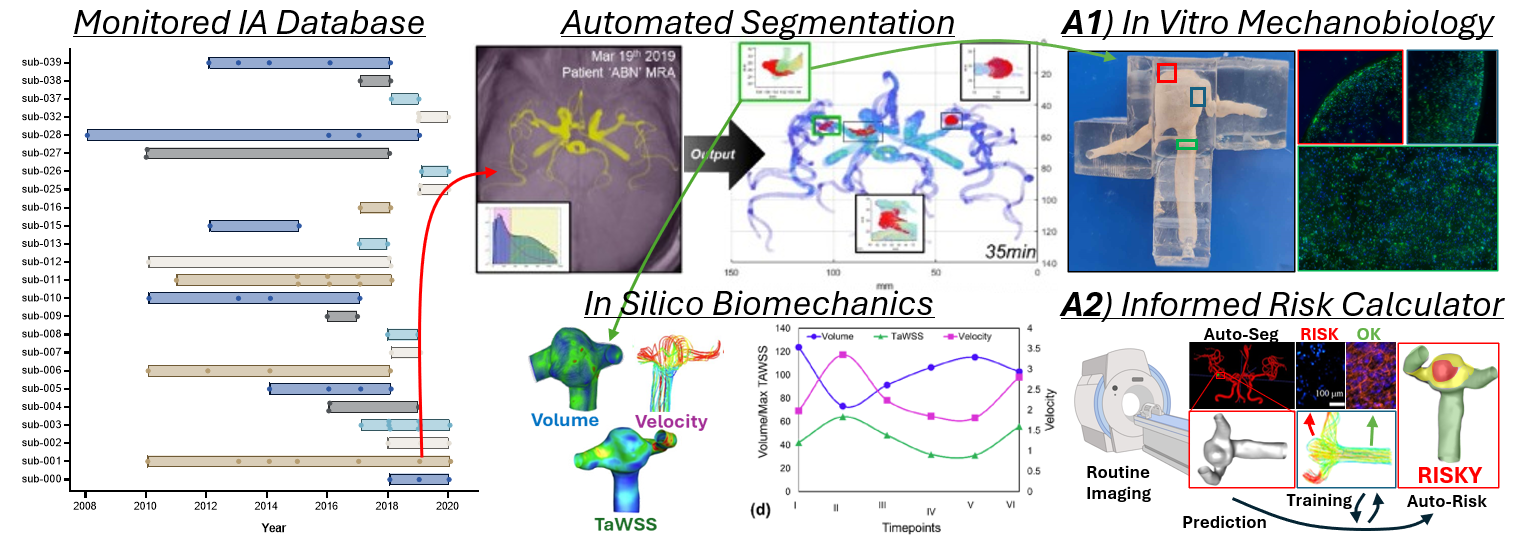
The ability to diagnose and medically or surgically treat cardiovascular disease is particularly dependent on the anatomy and biology of our body's vessels. Additive manufacturing leverages medical imaging, computational simulations, and 3D printing to fabricate patient-specific models of cardiovascular disease useful for identifying disease, predicting disease progression, or simulating treatments. Specifically, we are computationally simulating and 3D printing perfusable cell culture models to simulate intracranial aneurysm rupture risk and predict peripheral artery graft success.
Researchers: Chloe de Nys (Lead), Sabrina Schoenborn, Ryan McKinnon. Partners: Royal Brisbane & Women's Hospital Dept of Neurosurgery, Herston Biofabrication Institute, Princess Alexandra Hospital Dept of Vascular Surgery, Queensland University of Technology. Funding: Advance Queensland Industry Research Fellowship, Royal Brisbane & Women's Hospital Foundation, Bionics Gamechangers Australia, UQ Internal Funding.
If you are interested in collaborating with our lab in any of these focus areas or using our platform technologies toward new applications, please get in contact with Mark Allenby.

